Finally, there’s a light at the end of the tunnel.
The two pharmaceutical companies, Pfizer and Moderna, that have developed COVID-19 vaccines are reporting a 94% to 95% effectiveness rate—a beacon of hope in fighting the pandemic.
“94% to 95% efficacy is much higher than the annual influenza vaccine. Also, the high efficacy is maintained in the elder population. This is very promising,” says Dr. Mary Clance, epidemiologist with Luminis Health Anne Arundel Medical Center.
The Data
The New England Journal of Medicine reported on the results of Pfizer’s Phase 3 clinical trials late last month. A final analysis of its Phase 3 trial showed a 95% effectiveness rate. There were also no serious safety concerns.
The clinical trial has 43,548 participants enrolled. The company conducted trials in about 150 clinical sites in six countries, including 39 states.
The NEJM also reported on the results of Moderna’s Phase 3 clinical trials last month. Moderna’s data shows a 94.1% effectiveness rate at preventing severe disease from COVID-19. Moderna has 30,420 participants enrolled in the study at more than 100 clinical sites in the U.S.
Both Pfizer and Moderna have received emergency use authorization from the Federal Drug Administration (FDA), and began distribution of the vaccines last month.
The vaccines will continue to be monitored and studied. But so far, Dr. Clance and Jean Murray, director of Infection Control for Luminis Health Anne Arundel Medical Center, are very encouraged by the vaccines’ ability to prevent severe COVID disease.
What This Means
“Everybody is excited about the progress of the vaccine,” Jean says. “But, we need to remember that we still need to observe infection control precautions to prevent the spread of the disease until enough of the community is vaccinated.”
Remember to practice the 3Ws. Wash your hands, wear a mask and watch your distance. It’s going to take time to roll out the vaccine and immunize a significant number of the population.
“It’s not a magic bullet, so people will still need to continue to physically distance, wear a mask and wash their hands,” Jean says. “But the vaccine is an opportunity to give many, many more Americans immunity to prevent the spread of this virus.”
Questions Remain
But there are many unanswered questions. How long will a vaccine provide immunity? Can it be used in young children? When can the general public get the vaccine?
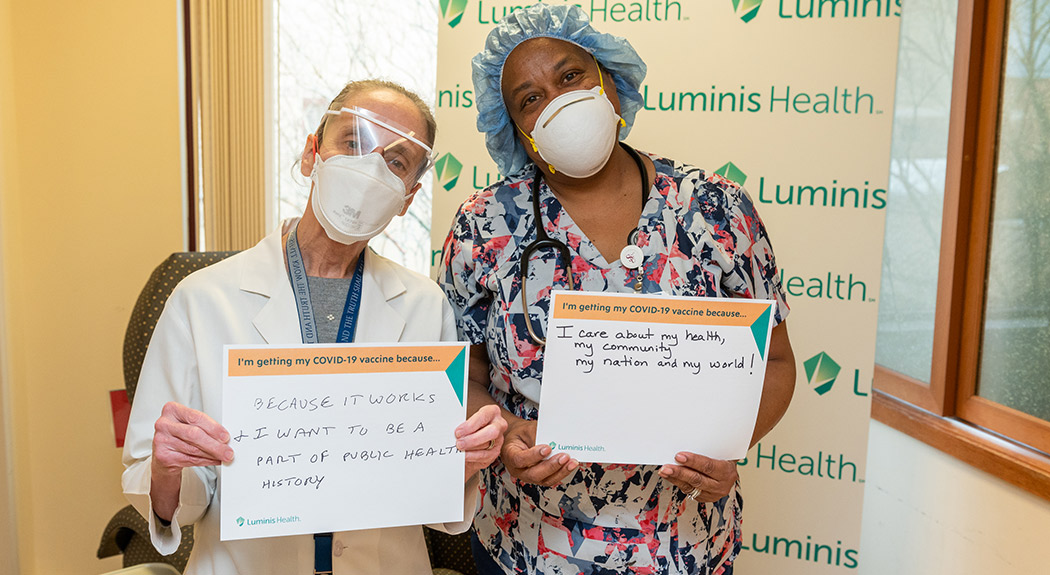
State health departments have developed plans to roll out the vaccine. Essential health care workers in hospital and nursing facilities were first to get it, followed by first responders including firefighters, police officers and emergency medical services personnel.
No vaccine is 100% effective, Dr. Clance says.
“The chances of getting COVID after vaccination with the two mRNA vaccines is very small,” she says. “The duration of immunity after vaccination is not yet known but will be learned in the months ahead with longer follow up of the past and current vaccine recipients.”
The Vaccine’s Effectiveness
The Centers for Disease Control and Prevention (CDC) say the trial data results are remarkable. Each year, the CDC looks at how well the flu vaccine protects against the flu. Recent studies show the flu vaccine reduces the risk of flu by between 30% and 60% among the overall population—compared to the 94% to 95% effectiveness the Pfizer and Moderna vaccines are showing against COVID. In some years the efficacy is much lower.
The challenge, Dr. Clance says, is that influenza viruses can change each year. The CDC anticipates which strains to target for the upcoming vaccine. Some years, the efficacy is lower because the vaccine doesn’t match the virus.
Coronaviruses, too, can mutate over time — as we are seeing with a more contagious strain recently discovered in the United Kingdom and now reported in several parts of the U.S.
We don’t yet know what percentage of the population will have to become immune to COVID to reach herd immunity – the point at which the virus runs out of bodies to infect because enough people have already gotten it.
How It Works
To best understand how the vaccine works, we need to describe how the virus works. The virus is transmitted via droplets into our nose, mouth or eyes. The virus then produces spike proteins. These spike proteins are used like a key in a lock. The key, or spike proteins, attaches and unlocks our cells to infect them and make more virus.
Both COVID-19 vaccines from Pfizer and Moderna were created using a genome sequence to design a molecule called messenger RNA (mRNA). The vaccine is not a live virus vaccine and cannot give COVID to those who receive it.
When the vaccine is injected, the mRNA in the vaccine instructs the cells to make the virus’ spike protein only. Our bodies recognizes these spike proteins as foreign and starts making antibodies, so when we are exposed in the future to the actual COVID virus, our bodies will immediately respond and defend us. The antibodies generated by the vaccine prevent viral attachment and infection.
Talk to Your Provider About the Vaccine
“We’re beginning a marathon here,” Dr. Clance says. “We want to tell the public to be patient, continue washing your hands, wearing a mask and watching your distance – and let this unfold.”
Talk to your doctor about when you could be eligible for the vaccine — and continue to follow Luminis Health for the latest updates.
Do you think you may have COVID-19? Check your symptoms here.